I want to add one more post after this one before we head home. It will be about the life of Jared Bangerter and how his story has blessed and influenced
our lives. But this post includes one last update for Levi for now and a thank you to
all who have served us in any way.
 |
| Wearing hat made by his Aunt Kristi |
Our community just recently had a fundraiser for
us that was headed up by my sister-in-
law. I want to share what my husband
posted on his Facebook in regards to this fundraiser and other service we have
received throughout this time. He expressed so eloquently how we
both feel. "We would like to express our deepest gratitude to all those
who took the time to put this fundraiser together and for all of those who
donated in any way. We have been very humbled by this experience and have been
so grateful for amazing friends, family and community members who have reached
out and showed their love and support, from those who have offered their time,
their home, helped with babysitting, offered donations, words of encouragement,
and most importantly, all of those who have been fasting and praying. We are
aware that there is a very real God out there that has answered those heart
felt prayers and it is nothing short of a miracle that little Levi is doing so
well. I know that there is a loving God who cares about the details of our
lives and that he looks down and touches our lives. There have been moments
that I was unsure if our son would make it through something like this, but
whether or not he did, the miracle of holding his tiny little body in my arms
and knowing that the Lord had blessed us with a child, was enough. Our hearts
go out to those who have dealt with this type of difficulty in their lives and
all those who deal with so much more. We have seen that there are people that
go through experiences far beyond what we are dealing with and they deal with
it so beautifully. We know that many of you have a silent untold story of your own, that you have
difficulties that others may never know about and we thank you for your prayers
and thoughts in spite of your own trials. We love you and pray that the Lord
will bless you all, for all you have done!"
 |
| Happy to be Eating and Sleeping like a Normal Baby! |
I am so grateful for the sacrifices and service
of others, but I often feel like Peter did when the Savior washed his apostles
feet when it comes to allowing others to serve me. But then I am reminded of
the Savior's instruction and important lesson to Peter as he washes his feet:
“5 …He
poureth water into a basin, and began to wash the disciples’ feet,
and to wipe them with the towel wherewith
he was girded.
8 Peter saith unto him, Thou needest not to wash
my feet. Jesus answered him, If I wash thee not, thou hast no part with me.
9 Simon
Peter saith unto him, Lord, not my feet only, but also my hands and my head.”
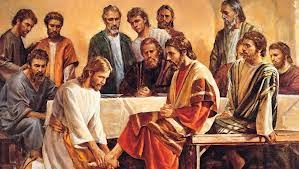 |
| The Savior washes Peter's feet |
I often feel like Peter did, that he should be washing the
Savior's feet or serving others, not the Savior serving him. But then the
Savior teaches Peter that we all have need of the Savior. The Lord often
blesses us or serves us through the lives of others. By allowing others to
serve us is like accepting the Savior into our lives and what He did for us,
whether we have temporal or spiritual needs. Likewise, as we reject the service
of others, we may be rejecting the Lord and denying the opportunity for others
to be blessed from the service they would have rendered. Another scripture
confirms this as it reads, "When ye are in the service of your fellow
beings, ye are only in the service of your God." We really could not have gone through this experience without the help of everyone. Thank you.






























